Prevention, diagnosis & management of dry eye in South Asia
Related content
Introduction
Dry eye is a condition that affects the tear film and affects the ocular surface that includes the conjunctiva and cornea.1 Dry eye, being a chronic disease, results in health related quality of life issues and economic problems due to loss of productive working days and the cost of medical treatment. Untreated dry eye may result in corneal surface ulceration and opacification leading to corneal blindness.
Definition of dry eye
In 2007, the International Dry Eye Workshop (DEWS) report defined dry eye as a multifactorial inflammatory disease of the tears and ocular surface, resulting in discomfort and visual disturbance, unstable tear film and ocular surface damage.1
Classification and Etiology
The dry eye condition is classified as evaporative dry eye and aqueous tear
deficient dry eye.2,3
Aqueous deficient dry eye is further subdivided as Sjogren syndrome dry eye and non-Sjogren dry eye.
Sjogren’s syndrome is a chronic inflammatory connective tissue disorder more common in females, who may be around 40 years of age. These patients may have dry eye and dry mouth. Primary Sjogren’s syndrome is without systemic disease;
Secondary Sjogren’s is with systemic disease.
Non-Sjogrens’s dry eye is seen in patients having Graft versus Host disease,
trachoma, conjunctival cicatrizing disorders and use of drugs such as antihistamines, decongestants, antipsychotic drugs, antidepressants and
antihypertensives.
Evaporative dry eye is most commonly caused by meibomian gland disease.
Epidemiology
Dry eye is more common in elderly females.4 Predisposing factors include collagen vascular disease, diabetes, allergy, antihistamines, pterygium and climate.4,5
Diagnosis of Dry eye
History taking, clinical examination followed by investigations are done to diagnose dry eye.
Symptoms
Patients with dry eye have a long history of symptoms such as of irritation and sandy or gritty sensation in the eyes. The symptoms may be mild to severe, and infrequent to long standing. The patients may have worsening of symptoms on prolonged visual work, intolerance to low humidity, feeling of dry eye and irritation. Dry eye is usually symptomatic although Sullivan et al have shown that 40% of patients having dry eye were asymptomatic and sometimes the symptoms may not correlate with the signs.6 There are various questionnaires such as Ocular surface disease index (OSDI score) and McMonnies questionnaire to identify, diagnose and manage dry eyes.7,8
Clinical examination
Observation of the lids, conjunctiva and cornea should be done first before
performing any test. The following is the sequence of examining a patient of dry eye.
1. Initial examination of lids and the ocular surface
2. TBUT – Tear film break up time after instillation of flurorescein dye
3. Corneal staining with fluorescein or lissamine green (between 1-4 minutes of lissamine green instillation)
4. The Schirmer 1 test (or phenol red thread test Schirmer test with anaesthesia) can be performed to determine the basal tear production. Tear osmolality should be measured after examination, if available.
Diagnostic tests
Schirmer test – The test is performed by putting a filter paper strip in the middle of lower fornix.9 After five minutes, the wetting of the filter strip is assessed. A wetting of 10mm or more is considered normal. Before applying a filter strip, excess tears should be wiped out otherwise the results may be showing a false high. Repeatability of this test and correlation with patient symptoms is poor.
Phenol red thread test – This test measures the tear volume. Phenol red, being pH sensitive, changes from red to yellow when exposed to tears.10 A 70mm thread is placed in lower fornix and wetting is measured after 15 seconds. The normal values range between 9mm-20mm and less than 9 mm is considered dry eye. Patel et al have shown that a value of 15 mm of wetting correlated with aqueous deficient and 22 mm with non-aqueous deficient dry
eye.11
Tear osmolality – This increases in patients with dry eye disease.
Tear film breakup time (TBUT)– A fluorescein strip is applied in the lower fornix and removed. The patient is asked to blink normally and then to stop blinking. The time taken from stopping blinking to the appearance of the first dark spot in the tear film indicates TBUT. A TBUT of <10 seconds is abnormal.
Videokeratography and keratometry– This can also can be used to assess the TBUT. Normal values for breaking of mires during keratometry are more than 15 seconds.
Meibography– Technological advances in the field of digital imaging have helped in assessing the meibomian glands, which if dysfunctional can result in evaporative dry eye. Various methods are available to do so including auto-refractometer.
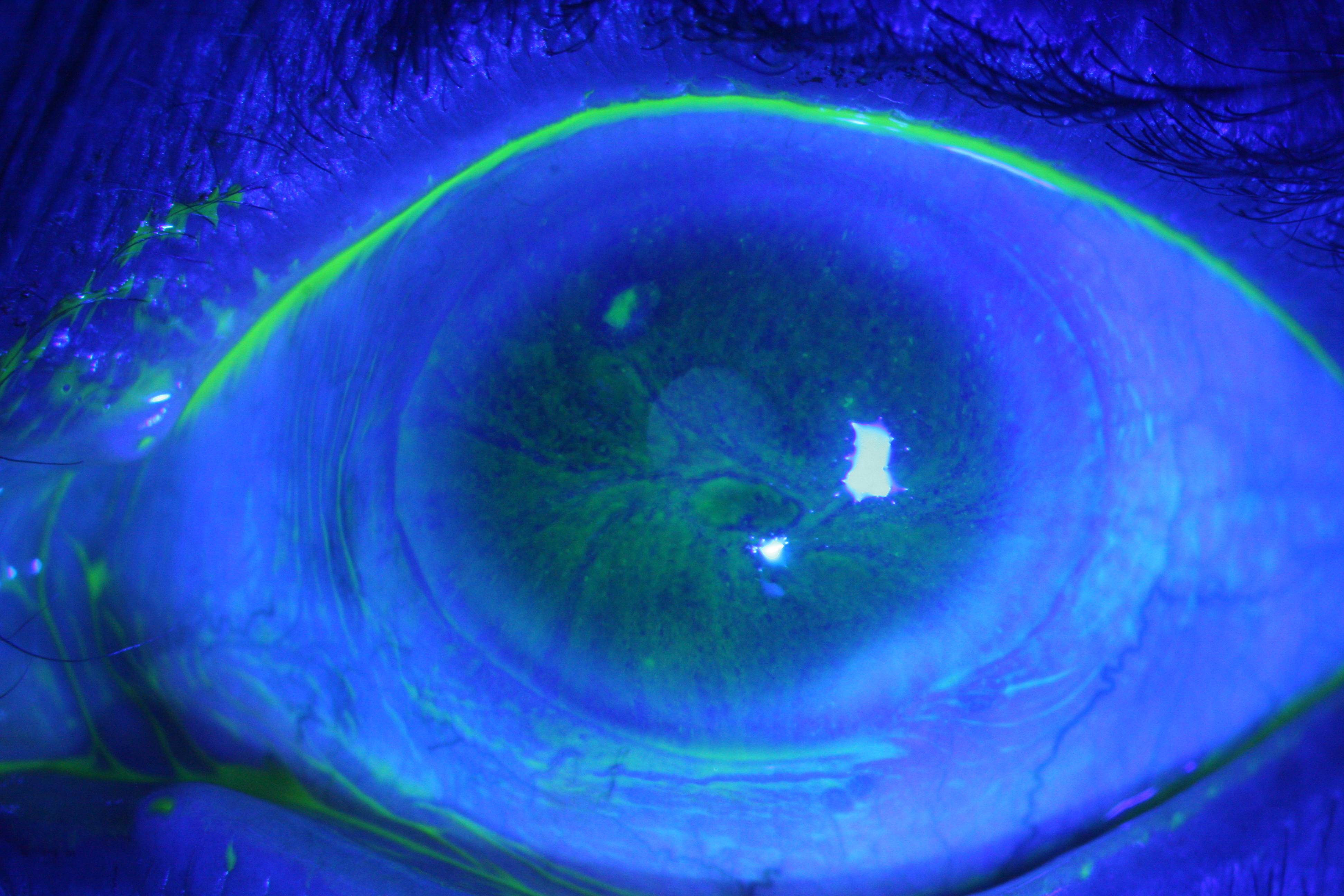
Corneal staining– Fluorescein staining of cornea appears greenish and is viewed using cobalt blue filter (Figure 1). The pattern of staining gives a clue to the etiology of dry eyes e.g. inferior corneal staining in patients having lagophthalmos or inability to close the eye lids; interpalpebral
staining in evaporative dry eyes.
Rose Bengal stain– It stains dead and devitalized cells of cornea and conjunctiva. The patients have severe stinging when Rose Bengal stain is used. One can also use lissamine green stain. Diagnosis is based on a combination of history, clinical examination and the investigations.
Management
Management depends on the severity of dry eye and response to the treatment.
Artificial tears and lubricating eye drops– This should be given to dry eye which is aqueous deficient. Artificial tears that merely increase tear volume may worsen symptoms in patients with a lipid deficiency.
Tear retention with Punctal occlusion– This may be indicated in patients who have symptomatic dry eyes, when Schirmer’s test is <5 mm and there is ocular surface staining. These can be done either with cautery or with punctal plugs (absorbable and non-absorbable).
Management of lids– Treat inflammation of the meibomian glands with hot bathing over closed eyelids followed by expression of the meibomian secretions. Use of lubricating eye drops, oral doxycycline and tetracycline may be helpful.
Key message
Dry eye is a multifactorial disease. It is important to determine whether it is aqueous deficient or evaporative dry eye or a combined one. Success of the treatment is dependent on proper understanding of the cause of dry eye and approach to the management.
Determination of tear meniscus height is important. Schirmer’s test will help differentiate aqueous deficient from evaporative dry eye. This should be done in all patients. Corneal staining with fluorescein, Rose Bengal and Lissamine green dyes will help assess damage to the ocular surface. Based on the level of damage, Schirmer’s test values and TBUT values, management can either be with lubricating eye drops, antiinflammatory agents, environmental modifications, or treatment of inflammation of the meibomian glands. The treating physicians should modify treatment based on patients’ symptoms.
References
4.Gayton JL. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 2009;3:405-12.
