Ocular surface injuries and management
Related content
Introduction
The term ‘ocular surface’ was first defined by Thoft in 1987 as a combined unit including the cornea, conjunctiva, lacrimal glands and eyelids. Gibson further described this term in 2007 to include the surface and glandular epithelia of the cornea, conjunctiva, lacrimal gland, accessory lacrimal glands, meibomian glands and the eyelashes with their associated glands of Moll and Zeis along with the nasolacrimal duct.1,2 These components of the ocular surface are connected with a continuous epithelium.
Being the most exposed part of the eye, the ocular surface is highly prone to
injury. This article covers the spectrum of various ocular surface injuries and their management.
Classification
Ocular surface injury is a broad term which includes the following:
• Ocular surface chemical and thermal burns or injuries
• Conjunctival laceration
• Corneal perforation
• Eyelid laceration
Ocular surface chemical and thermal burns
Ocular surface chemical and thermal burns Chemical injury may involve the ocular surface to a variable degree depending on the nature of the chemical agent, duration of exposure, concentration and volume of the agent. Host factors such as the nature and health of the ocular surface itself also plays an important role in deciding vulnerability of the surface to injury.
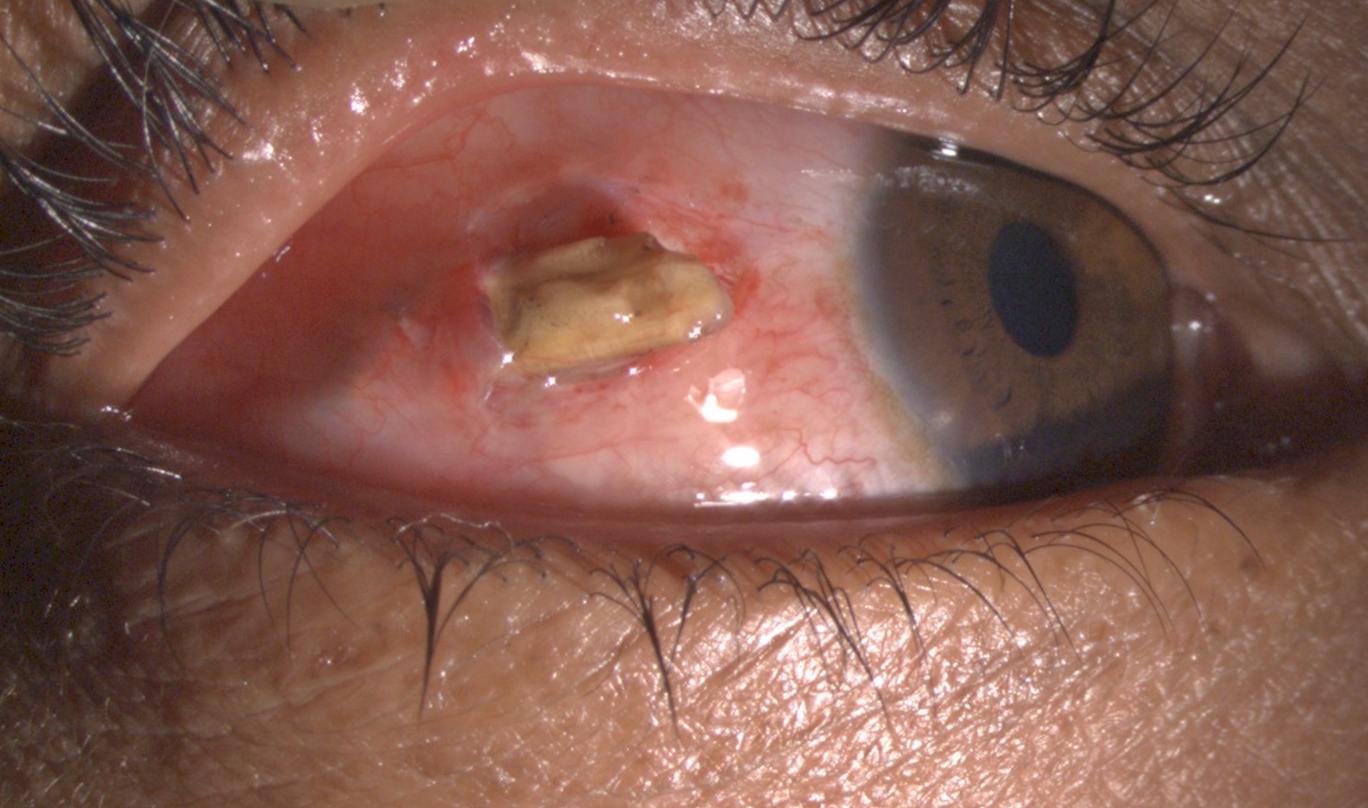
Figure 1. Clinical presentation of acute chemical injury



Most of the ocular surface chemical burns are due to either acids or alkalis.
Alkali burns account for two-thirds of these.3 A majority of these burns occurs in young males with increased risk of exposure to chemicals in the workplace.
Alkali burns-
The common alkaline sources include ammonia, lime or calcium hydroxide, lye or sodium hydroxide and magnesium hydroxide. The most common alkali causing ocular surface burns is lime while the most severe is ammonia. Ammonia, found in fertilizers and floor cleaners, has the most rapid penetration
into the surface due to its lipid as well as water solubility. Alkali burns are more severe than acid burns as they lead to saponification of cell membranes and intercellular bridges facilitating rapid penetration into the deeper layers and into aqueous and vitreous cavities. Alkali burns cause stimulation of nerve endings of cornea and conjunctiva and hence are more painful.5
Acid burns
Sulfuric acid is the most common acid implicated in acid induced ocular surface burns. Hydroflouric acid leads to the most severe burns as it is
highly reactive with rapid and deep penetration just like alkalis. Acids in
general cause less severe burns as compared to alkalis. They lead to coagulation and precipitation of proteins which in itself acts as a physical barrier, thus preventing further penetration of the agent.
Several classification systems have been suggested and proposed for ocular surface chemical injuries. Prominent ones include Hughes classification4 (1946), Roper-Hall classification5 (1965) and Dua’s classification6 (2001). These classification systems hold true for cases of acute chemical injuries. In chronic cases with already established sequelae of chemical burns, the ocular surface health may be graded using the Holland-Mannis classification system.
The two commonly used classification systems – Dua’s (2001) and Roper-Hall
(1964) are summarized in Table 1a and Table 1b.5,6 The Roper-Hall classification system has classified all burns with more than 50% limbal ischemia in Grade IV. This presents as a limitation in the prognostication
of the burns according to grade as the prognosis is highly variable in burns with just 50% limbal ischemia as compared to burns with total limbal ischemia. Dua’s classification in 2001 addressed this limitation and classified ocular surface chemical burns based on the clock hours of conjunctival and limbal involvement.7
Table 1a. Roper-Hall classification
| Grade | Prognosis | Cornea | Conjunctiva/ limbus |
|---|---|---|---|
| I | Good | Corneal epithelial damage | No limbal ischemia |
| II | Good | Corneal haze, iris details visible | 1/2 limbal ischemia |
| III | Guarded | Total epithelial loss, stromal haze, iris details obscured | 1/3-1/2 limbal ischemia |
| IV | Poor | Cornea opaque, iris and pupil obscured | >1/2 limbal ischemia |
Table 1b. Dua’s classification
| Grade | Prognosis | Clinical findings | Conjunctival involvement | Analogue scale |
|---|---|---|---|---|
| I | Very good | 0 clock hours limbal involvement | 0% | 0/0% |
| II | Good | ≤3 clock hours limbal involvement | ≤30% | 0.1-3/ 1-29.9% |
| III | Good | >3-6 clock hours limbal involvement | >30-50% | >3.1-6/ 31-50% |
| III | Good to guarded | 6-9 clock hours limbal involvement | 50-75% | >6.1-9/ 51-75% |
| III | Guarded to poor | 9-12 clock hours limbal involvement | >75-<100% | 9.1-11.9/ 75.1-99.9% |
| III | Very poor | Total (12 clock hours) limbal involvement | >100% | 12/100% |
| IV | Poor | Cornea opaque, iris and pupil obscured | >1/2 limbal ischemia |
Clinical features of ocular surface chemical burns- In the acute stage up to one week post injury, ocular surface chemical burns usually present with peri limbal ischemia (Figure 1a), corneal and conjunctival epithelial defects (Figure 1b) and retained chemical particles especially in the fornices (Figure 1c). Milder burns show re-epithelialisation gradually with or without treatment. More severe burns may develop complications such as persistent epithelial defects, dry eye, symblepharon, ankyloblepharon,cicatricial entropion or ectropion, and in rare and severe cases corneo scleral melt.8
Management of ocular surface chemical burns- Ocular surface chemical burn is a medical emergency. Immediate irrigation of the eye should be done with clean running water, ringer lactate or normal saline until the pH of the ocular surface is neutralized. This has to be meticulously done using double eversion of the eyelids.
Timely treatment should then be instituted. Medical treatment includes topical antibiotics, cycloplegics, topical steroids, topical sodium ascorbate 10%, topical sodium citrate 10%, oral doxycycline, oral ascorbate and tear substitutes.7
Amniotic membrane transplantation is beneficial in moderate to severe chemical burns. It promotes re-epithelialisation, decreases the incidence of symblepharon formation, and decreases inflammation.8
In chronic cases with already established limbal stem cell deficiency or
symblepharon formation, ocular surface rehabilitation may be required with symblepharon release with or without amniotic membrane transplantation.
Limbal stem cell transplantation may be done using fellow eye limbal stem cells or cadaveric limbal stem cells. Simple limbal epithelial transplantation (SLET) has been done with favourable outcomes in such cases (Figure 2a and Figure 2b)


Conjunctival laceration
Conjunctival laceration may occur following blunt or penetrating trauma. It presents with chemosis and subconjunctival hemorrhage. In such cases, it is important to rule out underlying scleral perforation. The fundus should be examined for any retinal tear or intraocular foreign body. An ultrasound may be done for the posterior segment evaluation. Such cases are managed with observation and topical antibiotics in mild cases and in large lacerations, surgical repair may be needed using 8-0 vicryl suture (Figure 3).

Corneal perforation
Corneal lacerations and perforations represent approximately 1 in 10 of ocular traumatic injuries presenting in an emergency medical setting. There may be associated adnexal injuries, and /or scleral perforation. The major goals of management of a corneal perforation are to remove any contaminants in the wound area, repair the tear and maintain the water tight integrity of the globe. Corneal perforation may also be associated with a foreign body (Figure 4).

Partial thickness lacerations may heal on their own with time. Such cases may require patching in the immediate phase followed by topical antibiotics. Full thickness lacerations may be repaired using interrupted 10-0 monofilament nylon sutures. In case of associated scleral involvement, the scleral wound should also be sutured using 6-0 vicryl suture. In case of uveal prolapse, the uveal tissue that is not necrotic and has protruded for less than 24 hours may be reposited back or and any old or necrotic prolapsed tissue carefully abscised. Other than conventional interrupted sutures, biological glue has also been used to seal the perforations especially those with tissue defect. Several studies have shown the beneficial effect of isobutyl cyanoacrylate glue for treatment of corneal perforations with tissue defect up to 3 mm.9,10
While suturing a corneal perforation, it is important to identify the major landmarks, especially limbus. It is advisable to preserve as much anatomy as possible and not over excise. The technique is to progressively halve the wound while passing sutures. They should be at 90% depth in the cornea. ‘No touch technique’ while passing sutures ensures a maintained anterior chamber during suturing. The central suture bites should be smaller and the length of suture should increase as one goes towards periphery.
For corneo scleral lacerations, it is important to perform a 360 degree peritomy and see the extent of scleral involvement, following which the limbus is secured with vicryl or monofilament nylon suture. Corneal sutures are placed as described above. Scleral wound is closed using ‘close as you go’ or zippering technique. Disinsertion and reinsertion of recti may be required in posterior tears.
Eyelid lacerations

Eyelids and lacrimal system are as much a part of the ocular surface as cornea and conjunctiva. Simple eyelid lacerations, which are horizontal follow skin lines and involve less than 25% of the lids, usually heal well even without suturing. Larger lid lacerations require surgical repair. Uncomplicated lid lacerations with no lacrimal system involvement can be repaired using interrupted silk sutures. In case of medial lid injuries (Figure 5) with damage to the lacrimal system, canalicular repair is required along with lid laceration repair.
Conclusion
Ocular surface injuries are fairly common owing to vulnerability of the exposed ocular surface to trauma. They range from ocular surface chemical burns, conjunctival laceration, corneal perforation and eyelid laceration. Effective and timely management of these types of injuries is essential for maintaining the integrity of the ocular surface.
References
3. Morgan SJ: Chemical burns of the eye: causes and management. Br J Ophthalmol 1987; 71:854-857.
5. Roper-Hall MJ. Thermal and chemical burns. Trans Ophthalmol Soc UK 1965;85:631–53
